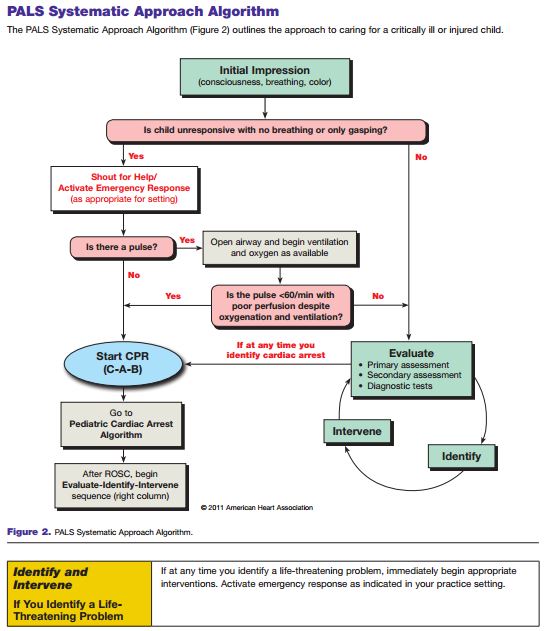
2015 Study Guide For Aha Bcls
In 2015, the AHA update to its Emergency Cardiovascular Care (ECC) guidelines strengthened some of the recommendations made in 2010. For an in-depth review of the changes made, refer to the AHA’s executive summary document.
Below are the details of the changes made to 2015 guidelines for BLS:. The change from the traditional ABC (Airway, Breathing, Compressions) sequence in 2010 to the CAB (Compressions, Airway, Breathing) sequence was confirmed in the 2015 guidelines.
The emphasis on early initiation of chest compressions without delay for airway assessment or rescue breathing has resulted in improved outcomes. Previously, rescuers may have been faced with the choice of leaving the individual to activate emergency medical services (EMS).
Now, rescuers are likely to have a cellular phone, often with speakerphone capabilities. The use of a speakerphone or other hands-free device allows the rescuer to continue rendering aid while communicating with the EMS dispatcher. Untrained rescuers should initiate hands-only CPR under the direction of the EMS dispatcher as soon as the individual is identified as unresponsive. Trained rescuers should continue to provide CPR with rescue breathing. In situations where unresponsiveness is thought to be from narcotic overdose, trained BLS rescuers may administer naloxone via the intranasal or intramuscular route, if the drug is available. For individuals without a pulse, this should be done after CPR is initiated.
The importance of high-quality chest compressions was confirmed, with enhanced recommendations for maximum rates and depths. Chest compressions should be delivered at a rate of 100 to 120 per minute, because compressions faster than 120 per minute may not allow for cardiac refill and reduce perfusion. Chest compressions should be delivered to adults at a depth between 2 to 2.4 inches (5 to 6 cm) because compressions at greater depths may result in injury to vital organs without increasing odds of survival. Chest compressions should be delivered to children (less than one year old) at a depth of one third the chest, usually about 1.5 to 2 inches (4 to 5 cm). Rescuers must allow for full chest recoil in between compressions to promote cardiac filling.
Because it is difficult to accurately judge quality of chest compressions, an audiovisual feedback device may be used to optimize delivery of CPR during resuscitation. Interruptions of chest compressions, including pre- and post-AED shocks should be as short as possible. Compression to ventilation ratio remains 30:2 for an individual without an advanced airway in place. Individuals with an advanced airway in place should receive uninterrupted chest compressions with ventilations being delivered at a rate of one every six seconds. In cardiac arrest, the defibrillator should be used as soon as possible. Chest compressions should be resumed as soon as a shock is delivered.
Biphasic defibrillators are more effective in terminating life-threatening rhythms and are preferred to older monophasic defibrillators. Energy settings vary by manufacturer, and the device specific guidelines should be followed. Standard dose epinephrine (1 mg every 3 to 5 min) is the preferred vasopressor. High dose epinephrine and vasopressin have not been shown to be more effective, and therefore, are not recommended.
2015 Study Guide For Getting Your Permit
For cardiac arrest that is suspected to be caused by coronary artery blockage, angiography should be performed emergently. Targeted temperature management should maintain a constant temperature between 32 to 36 degrees C for at least 24 hours in the hospital environment. Routine cooling of individuals in the prehospital environment is not recommended. Previously, the initial steps were Airway, Breathing, Compressions, or ABC. The literature indicates that starting compressions early in the process will increase survival rates. Therefore, the steps have been changed to Compressions, Airway, Breathing, or CAB.
This is intended to encourage early CPR and avoid bystanders interpreting agonal breathing as signs of life and withholding CPR. “Look, listen, and feel” for breathing is no longer recommended.
Instead of assessing the person’s breathing, begin CPR if the person is not breathing (or is only gasping for breath), has no pulse (or if you are unsure), or is unresponsive. Do not perform an initial assessment of respirations. The goal is early delivery of chest compressions to cardiac arrest persons.
High-quality CPR consists of the following:. Mathematical proofs second edition solutions manual pdf. Keep compression rate of 100 to 120 beats per minute for all persons. Keep compression depth between 2 to 2.4 inches for adults and children, and about 1.5 inches for infants. Allow complete chest recoil after each compression.
Minimize interruptions in CPR, except to use an AED or to change rescuer positions. Do not over ventilate. Provide CPR as a team when possible.
Cricoid pressure is no longer routinely performed. Pulse checks are shorter. Feel for a pulse for 10 seconds; if a pulse is absent or if you are not sure you feel a pulse, then begin compressions. Even trained clinicians cannot always reliably tell if they can feel a pulse. For infants, use a manual defibrillator if available. If not available, an AED with pediatric dose attenuator should be used for an infant. If an AED with dose attenuator is not available, then use an adult AED, even for an infant.